Allergic Rhinitis
Allergic Rhinitis – About
Allergic rhinitis, commonly known as hay fever, is a group of symptoms affecting the nose which occurs when your immune system overreacts to particles in the air that you breathe in and are allergic to. Your immune system mistakes an otherwise harmless substance as an invader and attacks the particles in your body, causing symptoms such as sneezing and a runny nose. The particles are called allergens, which simply means they can cause an allergic reaction.
People with allergies usually have symptoms for many years. There are two types of allergic rhinitis: Seasonal allergies means symptoms can occur in spring, summer and early fall. They are usually caused by sensitivity to airborne mold spores or to pollens from trees, grasses or weeds.
Perennial allergies means symptoms occur year-round and are generally caused by sensitivity to dust mites, pet hair or dander, cockroaches or mold.
The most common symptoms are: Stuffy nose due to blockage or congestion; Itching, usually in the nose, mouth, eyes, throat or skin; Puffy, swollen eyelids; Sneezing; Cough
You also may get other problems such as sinusitis and ear infections as a result of your allergies.
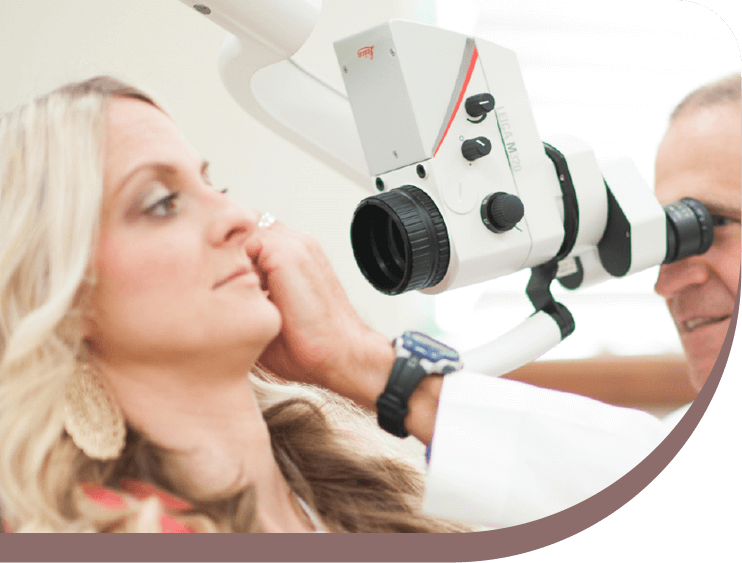
Allergic Rhinitis – Diagnosis
Allergic rhinitis is usually a long-standing condition that often goes undetected. Therefore, screening for rhinitis is recommended, particularly in asthmatic patients since studies have shown that rhinitis is present in up to 95% of patients with asthma.
The most common diagnostic tests for allergic rhinitis are the percutaneous skin test and the allergen-specific immunoglobulin E (IgE) antibody test. Less common diagnostic tools include nasal provocation testing, nasal cytology (e.g., blown secretions, scraping, lavage, biopsy), nasolaryngoscopy, and intra-dermal skin testing.
Skin testing involves introducing controlled amounts of allergen and control substances into the skin. Percutaneous testing is the most common type of skin testing and is preferred in primary care. It is convenient, safe, and widely accepted. Occasionally, intradermal testing is used (mostly by researchers and allergy subspecialists); it is more sensitive but less specific than percutaneous testing. It is unclear which method is superior; however, increased safety concerns exist with intradermal skin testing.
Allergic rhinitis can have an immediate or delayed response. Skin testing elicits both types of responses; however, the primary goal of skin testing is to detect the immediate allergic response caused by the release of mast cell or basophil IgE-specific mediators, which create the classic “wheal and flare” reaction after 15 minutes. The delayed response occurs four to eight hours after exposure to the sensitizing allergen and is less useful in clinical diagnosis.
Allergen-specific IgE antibody testing is particularly useful in primary care if percutaneous testing is not practical or if a patient is taking a medication that interferes with skin testing (e.g., tricyclic antidepressants, antihistamines).
Allergy testing in children has its own challenges. Authors of a large literature review provided evidence-based recommendations for allergy testing in children with various allergic diseases (e.g., rhinitis, asthma, food allergy). The review demonstrated that percutaneous skin testing is appropriate for children three years and older and that intradermal testing is appropriate at any age.
Allergic Rhinitis – Treatment
The main treatments for allergic rhinitis are avoiding allergens, managing symptoms with medicine and other home treatment, and, in some cases, getting immunotherapy (such as allergy shots). How often you need treatment depends on how often you have symptoms.
Avoid allergens
It is important to avoid allergens that are causing your symptoms. By doing this, you may be able to reduce your allergy symptoms and manage them without medicine or with fewer medicines.
You may need to clean your house often to get rid of dust, animal dander, or molds. Or you may need to stay indoors when pollen counts are high.
Manage symptoms
Taking medicines and doing other home treatments can help you manage your symptoms. For example, over-the-counter allergy medicines (such as antihistamines or decongestants) may help relieve some of your symptoms. They may come in the form of a pill, liquid, eye drops, or nasal spray. Or your doctor may prescribe stronger types of these medicines. You can do other things at home to help your symptoms, such as cleaning your nasal passages.
If medicines don’t help your symptoms or if they cause bad side effects, your doctor may suggest immunotherapy (allergy shots). Immunotherapy is a proven treatment approach providing long-term relief for many people suffering from allergic rhinitis. For this treatment, you get shots or use pills that have a small amount of certain allergens in them. Your body “gets used to” the allergen, so you react less to it over time. This kind of treatment may help prevent or reduce some allergy symptoms.
Another form of allergy immunotherapy recently approved in the United States is called sublingual immunotherapy (SLIT) allergy tablets. Rather than shots, allergy tablets involve administering the allergens under the tongue generally on a daily basis.
Sometimes people need surgery to fix a problem that makes treating allergies harder. You and your doctor should not consider surgery unless other treatments have failed.
Treatment for children
Treatment for children who have allergic rhinitis is much the same as for adults who have allergies. Treating children with medicine may be more difficult because of the possible side effects. Some medicines also may not be approved to treat children.
For outdoor allergies such as pollen, avoidance measures include limiting outdoor activities during times of high pollen counts. The National Allergy BureauTM (NAB) provides the most accurate and reliable pollen and mold levels from approximately 80 counting stations throughout the United States.
Your doctor might prescribe medication to decrease allergic rhinitis symptoms. These medications may include nasal corticosteroid sprays, antihistamine pills, nasal antihistamine sprays or decongestant pills. The majority of allergy medications for seasonal allergic rhinitis (hay fever) work best if started before pollen is in the air each spring and allergy symptoms develop. If you start taking allergy medications before you first come into contact with spring allergens, the medication can prevent the release of histamine and other chemicals. As a result, allergy symptoms are prevented from developing or are much less severe.
Conditions Treated
Follow us

Your Health Starts Here
"*" indicates required fields
