Microvascular Reconstruction
Microvascular Reconstruction – About
Microvascular reconstruction is a surgical procedure that involves moving a composite piece of tissue from another part of the body to the head and neck. The tissue most commonly comes from the arms, legs, or back, and can include bone, skin, fat, and/or muscle. The details of what is moved and where it is moved from are dependent on the reconstructive needs. Transfer of the tissue to the head and neck allows us to do things such as rebuild a jaw, optimize tongue function, or reconstruct the throat.
When these pieces of tissue are moved, they require their own blood supply for survival in their new location. This is similar to how an organ transplant works, except we are using a patient’s own body to provide the reconstructive tissue. After the transplanted tissue is carefully secured in the head and neck, the blood vessels that feed the tissue transplant are reconnected to new blood vessels in the neck. Since these blood vessels are usually 1 to 3 millimeters in diameter, the connections must be done with a microscope – hence, the term “microvascular surgery.”
This type of reconstruction may also be combined with other advanced surgical techniques, such as computer modeling, 3D printing, and customized implant fabrication. Prior to surgery, patients undergo careful assessment of functional impact and necessary rehabilitation planning.
Microvascular Reconstruction – Diagnosis
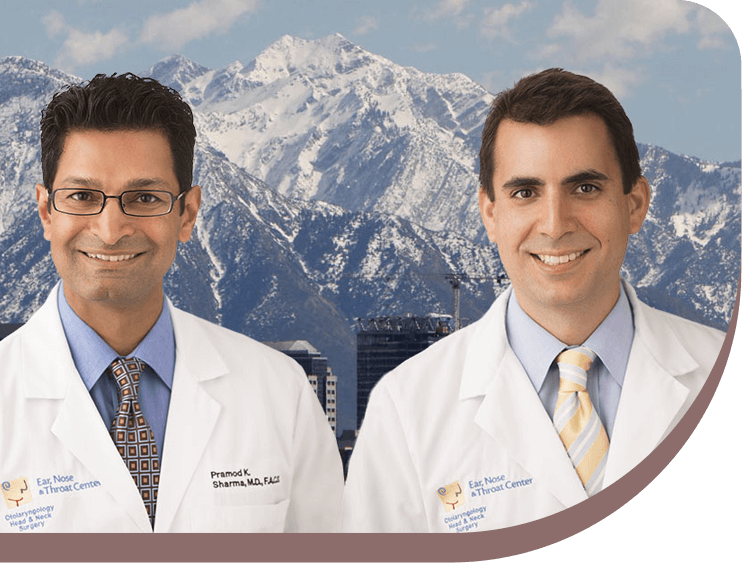
All patients referred to our Head & Neck Surgeons for resection of cancer are evaluated on the potential need for microvascular reconstruction. However, only a small group of patients will actually require it. The need for microvascular reconstruction depends upon the type of cancer surgery to be perfomed, the overall health of the patient, and a careful evaluation of potential functional and cosmetic changes from the cancer removal. For patients who have traumatic injuries or osteoradionecrosis (radiation damage to bone), microvascular surgery is occasionally necessary. If you have questions, ask to meet with a Head & Neck surgeon to discuss your options for treatment.
Microvascular Reconstruction – Treatment
Several types of microvascular reconstruction techniques may be used, including:
- Free muscle transfer — In this procedure, a surgeon harvests a muscle from the latissimus (back) or rectus abdominus (abdominal region) for reconstruction of the skull base or cranial vault. Muscle is particularly useful for sealing off the central nervous system and for promoting healing of complex wounds.
- Free bone transfer — Bony defects are often among the most difficult reconstructions as precise alignment of bone is required, as well as cutaneous (skin) coverage. Bone is most commonly used for mandibular reconstruction, but new innovation allows its use for midface and orbitomaxillary reconstruction. Donor sites for bony reconstruction include the fibula, scapula, iliac crest, and radial forearm.
- Free skin and free fat transfer — The radial forearm has long been the dominant flap used for cutaneous coverage. However, the anterolateral thigh flap is being used more in head and neck reconstruction because it has proven to be an ideal donor site with reliable vascularity, ease of harvest and versatility. Tissue types that may be safely harvested from this donor site include: skin, skin and fat, fat and fascia or fascia alone. The abundance of tissue available and the minimal morbidity from this site permits reconstruction of contour defects of the head and neck, pharyngeal reconstruction following laryngectomy, mucosalized tongue reconstruction and reconstruction of nasal lining and neck skin.
If the reconstruction is targeting your mouth, lower jaw bone, neck or throat, surgeons will often perform a temporary tracheotomy to ensure that your breathing will be safe. They may also place a temporary feeding tube to ensure that you may be fed while your wounds heal.
Recovery
After surgery, patients typically spend two days in the intensive care unit, followed by an additional three to five days in a regular hospital room before discharge. Patients will be assessed by physical therapy. In the event that there are extensive wound care or rehabilitation needs, they may be transferred to a rehabilitation hospital or be discharged with home nursing care.

Conditions Treated
Follow us

Your Health Starts Here
"*" indicates required fields
